The US Needs Therapy.
September 19, 2022
Our country is riddled with disease: The COVID pandemic, the Opioid epidemic, and the Monkeypox outbreak, just to name a few. To put it simply, our country is ill and things are further complicated when the illness is not easily identified by the human eye. Americans are more likely to be diagnosed with a mental illness at some point in their life than not. With millions of American children and adults in need of health care, the demand for mental health services is staggering. Clearly, there’s a demand, so what’s being done to ensure that every American in need of healthcare has access? The short answer is, not nearly enough.
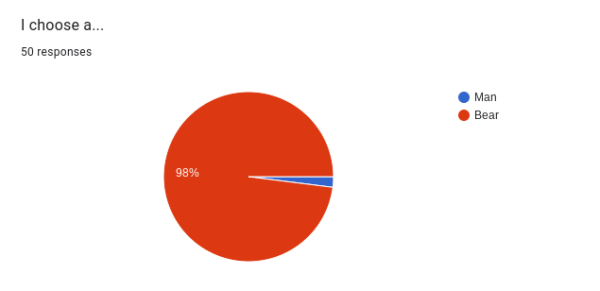
Most of us have been impacted negatively by mental health. Whether you’ve experienced mental illness yourself or have had a friend or family member affected, mental health is impossible to ignore. Having to coexist with Covid has only worsened our already strained system. At the height of the pandemic, 40% of US adults reported symptoms of depression or anxiety (compared to 11% pre-pandemic). That number has dropped to 33%, still lingering much higher than pre-pandemic numbers.
Let us imagine a not-so-distant world. Let’s imagine a country where one in four people have heart disease. In this same imaginary world, let’s imagine that the majority of counties in this country don’t have a single heart specialist and that 43% of those suffering don’t get treatment. This imaginary world is the reality for those living with mental illness in the good ole US of A. Not only are we sicker than ever, but for many, treatment is simply out of reach, with therapists being inaccessible for those in need of it.
Elena Charmichael, a first-year grad student at Penn State for clinical mental health counseling, is well aware of the difficulties and harm that can arise from a lack of access to mental health services. Originally from Franklin, Tennessee (just south of Nashville), Charmichael has seen firsthand the difficulties faced that are particular to rural areas.
With care providers spread out so far, many are forced to travel long distances to seek care. Unfortunately, when demand far exceeds supply, harmful practices and effects arise.
Carmichael described an equine mentorship program that was misrepresenting the services it offered.
“The fact that a lot of places that were mentorship programs said that they were therapy programs is actually, quite illegal, and it does way more harm than good,” Charmichael explained. “They’re not qualified to help clients that have been through trauma, or been through sexual abuse.” Many of these places are not licensed or trained properly, often providing “help” that is not only unhelpful, but damaging.
Elizabeth Toepfer, a Psychologist and Assistant Director of Counseling and Psychological Services at Penn State, expanded on some of the difficulties leading to this shortage.
“It’s a combination of both increased need and people willing to ask for help and there being more limitations on the number of people who are able to provide that help,” Toepfer said.
Many of the challenges arise from difficulties in getting people to enter the profession.
“There are some difficulties if you’re a professional of having to figure out what your pay is going to look like, what it’s going to look like working with insurance companies,” Toepfer explained.
While many people seek to help their clients and community, the hoops needed to jump through and management of outside forces can make providing the help that is so needed challenging and exhausting. Furthermore, the Covid pandemic, people’s personal lives, and more have led many to switch careers.
“We’re in the middle of a trend that is ‘people in professions are switching jobs,’ and anytime that that happens then that creates a disruption in being able to establish programs,” Toepfer said.
Continuity is key when it comes to treating mental health. Community efforts aimed at solving the current health crisis require consistency.
Even when those in need do have consistent help available, economic obstacles can make access to this help difficult. When the average psychotherapy session costs 100$-200$ without insurance, many find treatment to be, as Charmichael described,”so freaking expensive”, and simply out of reach.
“It costs so much just to exist,” Carmichael said. It’s true. As of June 2022, we’ve experienced the highest consumer price rise since November 1981. When the price to live is so high, many find their mental health being put on the back burner. “The majority of US citizens are looking at therapy and counseling as a luxury. Which it shouldn’t be. It’s a necessity,” she continued..
Elizabeth James, a mental health clinician at State High, further explained how counselor burnout and holes in the education system in general both contribute to the current shortage in schools. With counselors being pulled from their counseling positions to admin or other schools, we’ve experienced counselor changes every year.
“The whole education system itself is hurting which is where you see a lot of these turnover rates,” James said.
I myself have had 4 different counselors throughout high school–yet these are the people we are supposed to trust and have an established relationship with. Many students either don’t know who their counselor is or don’t even have one (some new counselors haven’t even arrived yet for the current school year).
It’s been shown that your relationship with your counselor or therapist is crucial to the effectiveness of the treatment.
“For therapy, 70% of success is just based on the relationship the therapist has with the client,” said James. She explained that the other 30% is based on techniques used, showing up to sessions regularly, and more. “A good counselor is like a pair of shoes, you either have one that fits perfectly or one you just need something different,” she explained.
From a student’s perspective, being able to open up to a stranger you might not be seeing consistently, is hard.
Sapphire Brown, a senior at Delta High, has a close relationship with the only counselor at the school. Having had the same person to go to for help since middle school has allowed her to establish a trusting and effective relationship.
“[My counselor] is very trained and she knows everything about me because I’ve known her for so long,” Brown explained.
As we all know, counselors are responsible for students’ schedules, college applications, and more in addition to counseling. This large workload can lead to students in need being put on a waitlist and waiting weeks to be seen.
“She’s doing a million other things[…]I’ve been sent over to State High before and the counselors just don’t know me,” said Brown.
Knowing that these counselors are not ones Brown will be seeing regularly limits how effective the visits are. “We’re just not able to connect in that way,” said Brown about her experience being deferred to different counselors.
But work is taking place. As far as State High goes, James’ position represents change. She was the first mental health clinician in SCASD and after realizing the value of her position, the district hired two more,one at the high school level and another at the elementary. James acts effectively as a bridge between in-school counseling and accessing care in the community.
To meet the current demand, we will no doubt need to explore some more…unconventional methods.
“The traditional way of just finding a therapist in a community where there are limitations really does create a challenge,” Toepfer said.
The pandemic saw the rise of telehealth as a way to allow people to continue receiving mental health services remotely. Telehealth allows for a counselor to serve a greater number of people, increasing the accessibility of the services.
“They could have clients from all over the state,” Toepfer explained and Carmichael agreed that telehealth can be a really good tool for attempting to solve the current shortage.
Telehealth isn’t without its limitations, however. During the peak of Covid, when people were moving back home, patients could continue to see their providers via telehealth over state lines. This has changed, Carmichael explained, creating a new host of challenges for those moving states. “That just really hinders how we can help,” Carmichael said. If you’ve found the perfect therapist that you really click with, leaving that completely is challenging.
“If they move you’re going to have to start over,” Carmichael said.
Of course, some people simply don’t want to talk to a screen.
“I couldn’t feel that connection because it’s not face to face, I was just telling all of my problems to a screen. It just didn’t feel like talking to an actual person,” Brown said when describing an appointment held remotely.
Despite the clear challenge, it’s evident that the conversation surrounding mental health is improving. Stigma is lessening and we as a country are starting to grasp its significance.
“It’s so cool to see the younger generation really fight for mental health,” Charmichael said. “It’s amazing how they’re not gonna take no for an answer.”
With more and more online tools being added, we can now access mental health resources in a matter of seconds. Undoubtedly, our treatment plan for our country will need to be creative, but its prognosis isn’t so bleak.